General Ophthalmology
Click on a topic to learn more: Cataracts | Contact Lenses | Dry Eye Care | Glaucoma | Routine Eye Care
Fairfax Eye Center is equipped with the latest technology in diagnostic and examination equipment. This allows us to provide our patients with the most thorough, comprehensive eye examinations available. Common diseases diagnosed and treated include Macular Degeneration, Dry Eye, Ocular Infections, Rosacea and other inflammatory diseases, Diabetic Retinopathy, Ocular Allergies, Pterygium, Flashes and Floaters.
We thoroughly check the internal and external health of your eyes including tests for cataracts and glaucoma. Dr. Hartzell also checks for the presence of corneal disorders and will examine the retina to ensure proper health and continued good vision.
Cataracts
 Cataract is a common condition that causes a clouding of the eye's natural lens. Cloudiness develops as a result of a buildup of protein in the lens fibers. Cataracts affect millions of people each year, including more than half of all Americans over the age of 65.
Cataract is a common condition that causes a clouding of the eye's natural lens. Cloudiness develops as a result of a buildup of protein in the lens fibers. Cataracts affect millions of people each year, including more than half of all Americans over the age of 65.
Cataracts cause a progressive, painless loss of vision. The lens clouds naturally as we age, causing patients to see a gradual reduction of vision. The causes of cataract are complex, including injury, certain medications, illnesses (such as diabetes), lifetime exposure to ultraviolet light, and smoking.
Symptoms of CataractsPatients with cataracts often do not experience any symptoms when the condition first develops. Cataracts will continue to progress with no apparent pain, although patients may experience:
- Blurred or hazy vision
- Double vision
- Poor vision in bright light
- Seeing halos around lights
- Poor vision at night
- Yellowish tinged vision
- Frequent changes in eyeglasses or contact lens prescription
- Trouble reading
If visual impairment begins to interfere with your ability to read, work, or do the things you enjoy, you may want to consider cataract surgery to restore your vision. Cataract surgery is the most commonly performed surgical procedure in the US. Surgery can be performed efficiently with a success rate of over 90 percent and a minimal risk of complications in most cases.
Cataract SurgeryCataract surgery is a minimally invasive procedure that involves numbing the eyes with anesthesia and then making a tiny incision into which an ultrasonic probe is inserted. The phacoemulsification probe breaks up, or emulsifies, the cloudy lens into tiny pieces and then suctions them out of the eye. Once the cloudy lens has been removed, a new artificial lens is implanted into the eye. This lens is known as an intraocular lens (IOL), and can often be inserted through the same incision.
Surgery usually takes less than 30 minutes to perform and is painless for most patients. After the procedure, a patch may be placed over the eye and you will be asked to rest for a while. Patients can return home the very same day, but will need someone to drive them home. For the next few days, you may experience itching, mild discomfort, mild discharge, and sensitivity to light and touch. Dr. Hartzell will prescribe eye drops to help the healing process and to reduce the risk of infection.
There are several different IOLs available to help each patient achieve the best possible results from his/her cataract surgery. Multifocal IOLs allow for full vision correction at near, intermediate and far distances, completely eliminating the need for eyeglasses or contact lenses in most patients. Some IOLs can also correct astigmatism.
These choices were not always available for cataract patients. In the past, cataract surgery only involved monofocal lenses, which could only focus on objects near or far, but could not adjust to accommodate varying distances. These patients still had to rely on glasses or contact lenses after surgery in order to see clearly at all distances.
Restor 3.0In December 2008, the latest IOL by AcrySof was approved for use in the US. The Restor 3.0 lens allows cataract replacement with +3.0 diopters add power at near, intermediate, and distance vision. Acrysof lenses have been the number one choice for cataract patients with presbyopia since they were introduced in 2005. This lens allows patients to enjoy improved comfort and vision for reading, computer work, and distance vision with the same safety and reliability as previous AcrySof lenses.
With the Restor 3.0 lens, most patients are satisfied with their vision after surgery, and many more were able to enjoy 20/20 vision at all three distances than with the previous Restor +4.0 D lens. Clinical results included a three-month follow-up exam showing that many patients would choose to have this lens implanted again.
ACRYSOF® ToricACRYSOF® Toric IOLs are used as a replacement lens in cataract surgery for patients with astigmatism. In addition to replacing the cloudy lens affected by cataracts, ACRYSOF®Toric IOLs correct astigmatism as well as nearsightedness or farsightedness. This lens also features an advanced aspheric option that improves image quality and increases contrast sensitivity. The ACRYSOF®Toric IOLs are a light yellow color that helps filter out blue light without affecting the color or quality of the patient's vision.
Although ACRYSOF®Toric IOLs are not accommodating and may still require eyeglasses or contacts to be worn, they offer many advantages to patients with astigmatism. Most patients report a high level of satisfaction with the ACRYSOF®Toric IOL lens, as it is the only lens to effectively treat astigmatism in cataract patients.
Risks and ComplicationsIf left untreated, cataracts will worsen over time and may lead to permanent vision loss or even blindness. It is important to have regular eye exams in order to detect cataracts as early as possible and to plan an effective treatment method.
Although cataract surgery is considered safe, there are certain risks associated with any surgery. Some of these risks may include pain, infection, swelling and bleeding. Most patients undergo this procedure without any complications.
Contact Lenses
 As a cornea specialist, Dr. Hartzell is uniquely qualified to safeguard the health of your corneas and determine if contact lens wear is right for you. Serious corneal infections and other sight-threatening complications can occur with contact lens wear. We require all of our contact lens patients to comply with a “wear and care” program individualized for each patient at the time of his or her contact lens exam.
As a cornea specialist, Dr. Hartzell is uniquely qualified to safeguard the health of your corneas and determine if contact lens wear is right for you. Serious corneal infections and other sight-threatening complications can occur with contact lens wear. We require all of our contact lens patients to comply with a “wear and care” program individualized for each patient at the time of his or her contact lens exam.
Dry Eye Care
 Dry eye occurs when the eye does not produce tears properly, or when the tears are not of the correct consistency and evaporate too quickly. In addition, inflammation on the surface of the eye may occur along with dry eye. If left untreated, this condition may cause sufferers to be unable to wear contact lenses and can lead to eye surface damage, pain, and vision problems over time. Dry eye can make normal activities such as driving, watching television, reading, or using a computer/tablet/smartphone very uncomfortable.
Dry eye occurs when the eye does not produce tears properly, or when the tears are not of the correct consistency and evaporate too quickly. In addition, inflammation on the surface of the eye may occur along with dry eye. If left untreated, this condition may cause sufferers to be unable to wear contact lenses and can lead to eye surface damage, pain, and vision problems over time. Dry eye can make normal activities such as driving, watching television, reading, or using a computer/tablet/smartphone very uncomfortable.
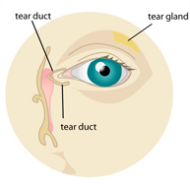
Tears, made by the lacrimal gland, are necessary for overall eye health and clear vision. Tears are made of proteins (including growth factors), electrolytes, and vitamins that are critical to maintain the health of the ocular surface and to prevent infection. Tears are in constant circulation and production can increase in response to insult (dust, wind, infection) in normal eyes. When the lacrimal gland fails to produce sufficient tears, dry eye can result. Any disease process that alters the components of tears can result in dry eye. People usually begin experiencing dry eye symptoms as they age, but the condition can also result from certain medications, conditions or injuries.
What are the symptoms of dry eye?Dry eye symptoms may include any of the following:
- Stinging or burning of the eye.
- A sandy or gritty feeling as if something is in the eye.
- Episodes of excess tears following very dry eye periods.
- A stringy discharge from the eye.
- Pain and redness of the eye.
- Episodes of blurred vision.
- Heavy eyelids.
- Uncomfortable contact lenses.
- Eye fatigue.
- Decreased tolerance of reading, working on the computer, or any activity that requires sustained visual attention.
What are the causes of dry eye?
Dry eye can be a temporary or chronic condition:
- Dry eye can be a side effect of some medications, including antihistamines, nasal decongestants,tranquilizers, certain blood pressure medicines, Parkinson's medications, birth control pills and anti-depressants.
- Skin disease on or around the eyelids can result in dry eye.
- Diseases of the glands in the eyelids, such as meibomian gland dysfunction, can cause dry eye.
- Dry eye can occur in women who are pregnant.
- Women who are on hormone replacement therapy may experience dry eye symptoms. Women taking only estrogen are 70 percent more likely to experience dry eye, whereas those taking estrogen and progesterone have a 30 percent increased risk of developing dry eye.
- Episodes of blurred vision.
- Dry eye can also develop after the refractive surgery known as LASIK. These symptoms generally last three to six months, but may last longer in some cases.
- Dry eye can result from chemical and thermal burns.
- Allergies can be associated with dry eye.
- Infrequent blinking, associated with staring at computer or video screens, may also lead to dry eye symptoms.
- Loss of sensation in the cornea from long-term contact lens wear can lead to dry eye.
- Dry eye can be associated with immune system disorders such as Sjögren's syndrome, Lupus, and Rheumatoid Arthritis. Sjögren's leads to inflammation and dryness of the mouth, eyes, and other mucous membranes. It can also affect other organs, including the kidneys, lungs and blood vessels.
- Dry eye can be a symptom of chronic inflammation of the conjunctiva or the lacrimal gland both of which can be caused by certain eye diseases, infection, exposure to irritants such as chemical fumes and tobacco smoke, or drafts from air conditioning or heating.
- If the surface area of the eye is increased, as in thyroid disease when the eye protrudes forward or after cosmetic surgery if the eyelids are opened too widely, dry eye can result.
- Dry eye may occur from exposure keratitis, in which the eyelids do not close completely during sleep.
How is dry eye treated?
Dry eye must be managed as an ongoing condition. The first priority is to determine if an underlying disease is the cause of dry eye (such as Sjögren's syndrome or lacrimal and meibomian gland dysfunction). Dr. Hartzell has established a Dry Eye Center of Excellence to bring the newest and most advanced diagnostic techniques to her patients in Northern Virginia. Rapid, accurate diagnosis, will lead to more efficient and successful treatment. Testing may include the Sjo bloodtest and the RPS InflammaDry Detector.
SjöTM
 SjöTM is a laboratory test for the diagnosis of Sjögren’s Syndrome in patients with dry eye symptoms, available in the US. SjöTM is currently not available in Europe or the rest of the world.
SjöTM is a laboratory test for the diagnosis of Sjögren’s Syndrome in patients with dry eye symptoms, available in the US. SjöTM is currently not available in Europe or the rest of the world.
InflammaDry® is the first and only, rapid, in-office test that detects MMP-9, an inflammatory marker that is consistently elevated in the tears of patients with dry eye disease.
Depending on the causes of your dry eye, Dr. Hartzell may use various approaches to treat your disease.
- Artificial tears, gels, and ointments - available over the counter - as the first line of therapy. These agents offer temporary relief and provide an important replacement of naturally produced tears in patients with aqueous tear deficiency. Avoid artificial tears with preservatives if you need to apply them more than four times a day or preparations with chemicals that cause blood vessels to constrict.
- Wearing glasses or sunglasses that fit close to the face or that have side shields can help slow tear evaporation from the ocular surface. Indoors, an air cleaner to filter dust and other particles helps prevent dry eyes. A humidifier also may help by adding moisture to the air.
- Avoid dry conditions and allow your eyes to rest when performing activities that require you to use your eyes for long periods of time. Instill lubricating eye drops while performing these tasks.
Cyclosporine (Restasis), an anti-inflammatory medication, is the only prescription drug available to treat dry eye. It decreases corneal damage, increases tear production, and reduces symptoms of dry eye. It may take three to six weeks for Restasis to take effect and three months before achieving the full benefit of this medication. In some cases of severe dry eye, short term use of corticosteroid eye drops is also required.
If dry eye results from taking a medication, Dr. Hartzell may recommend switching to a medication that does not cause the dry eye side effect.
If contact lens wear is a problem, Dr. Hartzell may recommend another type of lens or reducing the number of hours you wear your lenses.
Additional therapy includes punctal plugs. These are tiny silicone inserts placed into the tear drainage openings at the inner corner of the eyelids where tears drain from the eye into the nose. Insertion is painless and performed by Dr. Hartzell in her office. In severe dry eye cases, permanent closure of the puncta may be required.
In some patients with dry eye, supplements or dietary sources (such as tuna fish) of omega-3 fatty acids (especially DHA and EPA) may decrease symptoms of irritation. The use and dosage of nutritional supplements and vitamins should be discussed with your primary medical doctor.
Glaucoma
 Glaucoma is the leading cause of blindness and visual impairment in the United States. A simple eye exam can detect the disease. With early detection and treatment, glaucoma can usually be controlled and blindness prevented.
Glaucoma is the leading cause of blindness and visual impairment in the United States. A simple eye exam can detect the disease. With early detection and treatment, glaucoma can usually be controlled and blindness prevented.
Glaucoma can affect anyone from newborn infants to the elderly. It has been estimated that up to 3 million Americans have glaucoma. At least half of those people do not know they have the disease. People who are at greater risk for glaucoma usually have one or more of the following conditions:
- At Least 45 Years Old Without Regular Eye Exams
- A Family History of Glaucoma
- Abnormally High Eye Pressure
- African American Descent
- Nearsightedness
- Diabetes
- Previous Eye Injury
- Regular, Long-term Use of Cortisone/Steroid Products
To detect glaucoma, Dr. Hartzell will test your visual acuity, visual field, dilate your pupils and test the pressure in your eye. Regular and complete eye exams help to monitor the changes in your eyesight and will help to determine whether you may develop glaucoma.
Treatments to control glaucoma include medications, laser surgery and conventional surgery.


